Background: CAR T cells and TCE are approved for the treatment of RRMM and are being investigated in newly diagnosed pts. Because their mode of action differs with respect to other drugs used in MM, the clinical significance of conventional prognostic factors must be reanalyzed in the era of newer immunotherapies. In this regard, the role of MRD remains uncertain in RRMM pts treated with CAR T cells, and virtually unknown in the setting of TCE.
Aim: Analyze the clinical significance of MRD assessment in RRMM pts treated with CAR T cells and TCE.
Methods: This study included 269 RRMM pts, 125 treated with CAR T cells and 144 with TCE. Most pts received anti-BCMA (n=193) and anti-GPRC5D (n=55) immunotherapies. The median follow-up was 11 months. MRD was assessed in bone marrow aspirates from 190 of the 269 RRMM patients; those without an assessment were considered as MRD positive in the intent to treat (ITT) analyses. A total of 509 longitudinal MRD studies were performed using NGF in the core laboratories of PETHEMA/GEM. The median number of MRD studies per pt was 2 (range, 1 - 7) High-risk cytogenetics included t(4;14), t(14;16) and/or del(17p). Extramedullary disease (EMD) was considered if involving soft tissues.
Results: Pts treated with CAR T cells and TCE received a median number of three and four prior lines of therapy, respectively. Those infused with CAR T cells had more frequently ISS 1 (57% vs 40%, P = .02) and showed less EMD (23% vs 40%, P = .006) compared to cases treated with TCE. The incidence of high-risk cytogenetics was similar in both groups. The median PFS and OS of the ITT population since treatment initiation was 10 and 25 months, respectively.
The median PFS of MRD negative (n=122, 45%) vs MRD positive (n=147, 55%) pts was 20 vs 3 months (HR: 0.11, P <.001). The median OS was not reached vs 7 months, respectively (HR: 0.16, P <.001). The longitudinal MRD assessments showed significant differences in survival outcomes between pts with sustained MRD negativity (n=91) vs those converting from MRD negative to positive (n=28) vs those who never attained MRD negativity (n=122). The median PFS was 38 vs 12 vs 3 months ( P <.001), and the rates of OS at 2 years were 84%, 57% and 25% ( P <.001), respectively. The percentage of pts with more than one (n=102), two (n=58) or three (n=27) MRD negative results who relapsed was 35%, 29% and 22%, respectively.
In the ITT population, MRD negative rates were significantly higher in pts treated with CAR T vs TCE (78% vs 35%, P < .001). The MRD negative rates with CAR T vs TCE at the 6-, 12- and 24-month landmark were 66% vs 29% ( P < .001), 45% vs 19% ( P < .001) and 25% vs 9% ( P = .01). The superior MRD negative rates with CAR T vs TCE were observed in pts previously exposed to >3 lines of therapy (63% vs 31%, P < .001), with ISS 3 (47% vs 21% P = .08), high risk cytogenetics (73% vs 30%, P < .001) and EMD (68% vs 30%, P = .001). There were no differences in the PFS and OS of MRD negative and MRD positive patients when stratified according to CAR T vs TCE treatment.
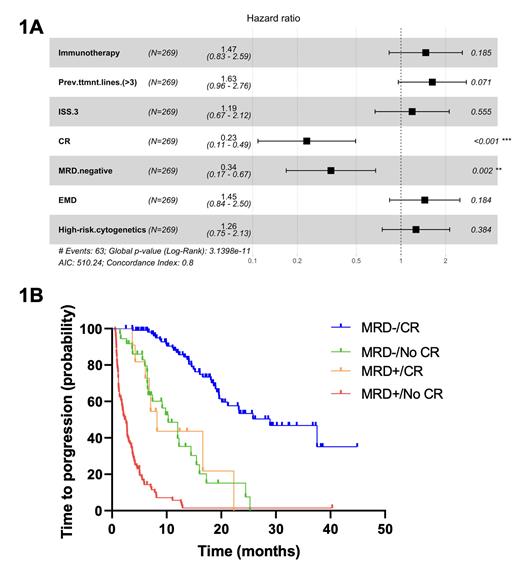
Among MRD negative pts, those previously exposed to > 3 lines of therapy and with ISS 3 showed inferior outcomes. By contrast, the presence of high-risk cytogenetics and EMD were not associated with inferior PFS and OS in MRD negative pts. In a multivariate analysis including the number of prior lines of therapy, CAR T vs TCE therapy, ISS, cytogenetic risk, EMD, CR and the MRD status, the latter was an independent prognostic factor of PFS (HR: 0.19, P < .001) and OS (HR: 0.34, P = .002). The CR status also retained significance while the other prognostic factors did not (Fig 1A).
Because of the independent prognostic value of the CR and MRD status, pts were stratified as MRD-/CR (n=110), MRD-/NoCR (n=36), MRD+/CR (n=11) and MRD+/NoCR (n=105). The respective median PFS was 29, 10, 8 and 2 months ( P < .001) (Fig 1B). The respective OS rates at 2-years were 84%, 36%, 58% and 18% ( P < .001).
Conclusions: Achieving sustained MRD negativity resulted in significantly prolonged survival of RRMM pts treated with newer immunotherapies. While MRD negative rates were superior in those eligible to CAR T cells vs TCE, the impact of achieving MRD negativity in pt' survival was similar in both settings.
In contrast to newly-diagnosed MM, achieving CR does matter in MRD negative RRMM pts with respect to response durability after CAR T cells and TCE. Accordingly, depth of response determined by CR and undetectable MRD was the most relevant prognostic factor and should be considered as the treatment endpoint in this setting.
Disclosures
Puig:Janssen: Consultancy, Honoraria, Other, Research Funding; Sanofi: Consultancy, Honoraria; The Binding Site: Consultancy, Honoraria; Takeda: Consultancy, Honoraria, Other, Research Funding; BMS: Consultancy, Honoraria, Other, Research Funding, Speakers Bureau; Amgen: Consultancy, Honoraria, Other, Research Funding; Pfizer: Research Funding. Rodriguez Otero:Regeneron: Other: Honoraria for lectures; Janssen: Consultancy, Membership on an entity's Board of Directors or advisory committees, Other: Honoraria for lectures; AbbVie: Consultancy, Membership on an entity's Board of Directors or advisory committees; Oncopeptides: Membership on an entity's Board of Directors or advisory committees; Pfizer: Consultancy, Membership on an entity's Board of Directors or advisory committees, Other: Travel grants; Amgen: Other: Honoraria for lectures; Bristol Myers Squibb: Consultancy, Membership on an entity's Board of Directors or advisory committees, Other: Honoraria for lectures; GlaxoSmithKline: Membership on an entity's Board of Directors or advisory committees, Other: Honoraria for lectures; Sanofi: Membership on an entity's Board of Directors or advisory committees, Other: Honoraria for lectures; Roche: Consultancy. Gonzalez-Calle:Prothena: Consultancy; BMS: Honoraria; Janssen: Consultancy, Honoraria, Research Funding. Lopez Corral:Novartis: Honoraria, Other: travel support; Gilead Sciences: Honoraria, Other: travel support; Janssen: Honoraria, Other: travel support. Mateos:Amgen: Honoraria; GSK: Honoraria, Membership on an entity's Board of Directors or advisory committees; BMS-Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees; Janssen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Takeda: Honoraria; Regeneron: Honoraria; Pfizer: Honoraria, Membership on an entity's Board of Directors or advisory committees; Sanofi: Honoraria, Membership on an entity's Board of Directors or advisory committees; Oncopeptides: Honoraria, Membership on an entity's Board of Directors or advisory committees; Abbvie: Honoraria, Membership on an entity's Board of Directors or advisory committees; University of Salamanca/Gerencia Regional de Salud de Castilla y León: Current Employment; Stemline: Honoraria, Membership on an entity's Board of Directors or advisory committees. San-Miguel:Regeneron: Other: Advisory Board; Haemalogix: Other: Advisory Board; Takeda: Other: Advisory Board; MSD: Other: Advisory Board; Janssen-Cilag: Other: Advisory Board; GSK: Other: Advisory Board; Celgene: Other: Advisory Board; BMS: Other: Advisory Board; Amgen: Consultancy, Other: Advisory Board; Abbvie: Consultancy, Other: Advisory Board; Roche: Other: Advisory Board; Karyopharm: Other: Advisory Board; Novartis: Other; Sanofi: Other: Advisory Board; SecuraBio: Other: Advisory Board. Paiva:Adaptive: Honoraria; Bristol-Myers Squibb: Consultancy, Honoraria, Research Funding; Roche Glycart AG: Honoraria, Research Funding; Janssen: Consultancy, Honoraria; Sanofi: Consultancy, Honoraria, Research Funding; EngMab: Research Funding; GSK: Honoraria, Research Funding; Takeda: Honoraria, Research Funding; Amgen: Honoraria; Gilead: Honoraria; Oncopeptides: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal